Over half the global population has been infected with H. pylori, the most widespread bacterial infection in the world (1, 2). Even in developed countries, where overall infection levels have been declining, physicians encounter high prevalence rates, which are even greater among immigrant and economically disadvantaged patients. Serology testing is a common way to detect H. pylori antibodies, but as patients can remain seropositive for many years following an infection, are not useful in determining current disease. How then can diagnosis and treatment decisions be made?
H. pylori Pathology
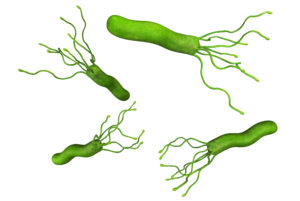
H. pylori is typically acquired in childhood. If left untreated, it persists and remains transmissible for the lifetime of the patient (3, 4). Prevalence rates increase with age, but lower rates of H. pylori infection in children reflects recent improvements in control and transmission in the young. Transmission between family members is frequent (1, 4), with grandparents a common, unsuspecting source of infection (5).
Symptoms of H. pylori infection initially include pain in the stomach or upper abdomen. The bacteria penetrate the protective gastric mucous to trigger irritation, neutrophil invasion, and inflammation of the gastric surface, leading to gastritis (6). It is not known what portion of exposed individuals escape or suppress active inflammation, but for those with persistent colonization, gastritis and acid secretion set the stage for further complications (7).
In 10-20% of infected patients, chronic and active inflammation lead to the subsequent development of peptic ulcers (6). For patients with intact acid secretion, H. pylori will be more abundant and tissue inflammation more prominent in the gastric antrum with fewer bacteria and less inflammation in the corpus (6). These patients are more likely to develop antral and duodenal ulcers. Previously, H. pylori infection was responsible for 90% of duodenal ulcers and 80% of gastric ulcers (1). Currently, in developed countries, although H. pylori infections are decreasing, an increasing portion of peptic ulcer disease is linked to use of non-steroidal anti-inflammatory drugs (NSAIDs) (1, 8). Patients who are considering long-term NSAID therapy should be tested for H. pylori infection, as the combination further increases the risk of ulcer development (9). This changing incidence emphasizes the importance of correct diagnosis of dyspepsia and ulcerations to differentiate disease caused by drugs from disease caused by H. pylori infection.
Patients with low acid secretion, notably those taking proton pump inhibitors (PPIs), can develop gastritis throughout the stomach, with ulcers occurring where inflammation is most severe (6). Complications of ulcers are serious, including bleeding, perforation, and strictures. If bleeding ulcers are caused by H. pylori, there is a high risk of recurrence; antibiotic therapy to eradicate the bacteria is usually successful and reduces this risk (6). When low acid secretion allows inflammation to remain chronically active, patients can develop metaplasia and, eventually, inflammation-induced gastric cancers. Atrophic gastritis is a precursor to gastric cancer and decreases acid secretion even further (10).
General H. pylori infection is associated with a 2-3 fold increased risk of gastric cancer or mucosal associated-lymphoid-type (MALT) lymphoma (1). Stomach cancers were previously a common type of cancer in the United States. In parallel with the decreasing incidence of H. pylori infections, stomach cancers have declined and are estimated to be the 15th most common cancer in the USA. Nevertheless, 5-year overall survival rates are only 31% and 10,800 people in the USA and over 700,000 people globally die from stomach cancer annually (1, 9, 11). For the 35% of patients who have metastatic disease, the relative 5-year survival is only 5% (11). Because H. pylori colonization is the single biggest risk factor for stomach cancer (1) and because the bacteria are classified as a Class I carcinogen, diagnosis of infection is clinically important.
H. pylori Treatment
The ability to treat and cure H. pylori infections with antibiotics has revolutionized clinical care of patients and reversed long-standing disease trends. Improving what had been a life-long, deteriorating condition, eradication of H. pylori decreases inflammation, and if therapy is given before atrophic changes occur, even the risk of cancer can be virtually abolished (10).
 There are multiple therapies that can be successful (12). Triple therapy is widely used and consists of a PPI, amoxicillin and clarithromycin for 10-14 days (9). Sequential therapy utilizes amoxicillin plus a PPI for the first 5 days then moves to a triple therapy of a PPI and two antibiotics, such as clarithromycin and tinidazole (9). Eradication of H. pylori is becoming more difficult due to increasing resistance of H. pylori strains to clarithromycin, making these treatments less effective (13). Recent studies show that clarithromycin resistance is 32% in the USA and 50% in Japan (4), while metronidazole resistance in Africa is over 90% (9). As a result, the AGC 2017 Guidelines suggest using treatment regimens without clarithromycin if local resistance rates exceed 20% (3). This resistance has led to development of a quadruple therapy that uses a PPI, a bismuth product and antibiotics such as metronidazole and tetracycline for 10-14 days (9). However, for H. pylori-infected patients who are pregnant, bismuth, tetracycline and fluoroquinolones are potential teratogens and should be avoided (9).
There are multiple therapies that can be successful (12). Triple therapy is widely used and consists of a PPI, amoxicillin and clarithromycin for 10-14 days (9). Sequential therapy utilizes amoxicillin plus a PPI for the first 5 days then moves to a triple therapy of a PPI and two antibiotics, such as clarithromycin and tinidazole (9). Eradication of H. pylori is becoming more difficult due to increasing resistance of H. pylori strains to clarithromycin, making these treatments less effective (13). Recent studies show that clarithromycin resistance is 32% in the USA and 50% in Japan (4), while metronidazole resistance in Africa is over 90% (9). As a result, the AGC 2017 Guidelines suggest using treatment regimens without clarithromycin if local resistance rates exceed 20% (3). This resistance has led to development of a quadruple therapy that uses a PPI, a bismuth product and antibiotics such as metronidazole and tetracycline for 10-14 days (9). However, for H. pylori-infected patients who are pregnant, bismuth, tetracycline and fluoroquinolones are potential teratogens and should be avoided (9).
Because of antibiotic resistance, attempts to eliminate H. pylori with these regimens have increasing failure rates and eradication can no longer be assumed. Elimination of the bacteria should be confirmed 4 weeks after the treatment is finished, using a test such as a stool antigen assay, rather than a serology test (antibodies to H. pylori are formed within 3 weeks post-infection) (9). Guidelines recommend follow-up testing four weeks post-treatment as this time-frame allows any surviving H. pylori to re-grow to detectable levels (3).
H. pylori Diagnosis
Multiple professional gastroenterology groups have endorsed a “Test-Treat-Test” approach that involves first using a non-invasive diagnostic test to determine if a patient with dyspepsia is infected with H. pylori, treatment if infection is present, then follow-up testing to confirm removal of the bacteria (3, 7, 12). For patients this prevents the expense, inconvenience, and discomfort of endoscopy. For physicians, diagnosis can be rapid, and therapy initiated with confidence.
H. pylori infections and associated symptoms and inflammation can wax and wane. Patients typically seek medical care for troubling symptoms during a period of active inflammation. If H. pylori diagnostic testing is positive, they should receive eradication treatment to prevent worsening disease and to potentially reverse and heal their current lesions. The AGC 2017 Guidelines indicate that if a physician plans to test a patient for H. pylori then the patient should be treated if positive (3). The fundamental decision then, is not whether to treat, but rather what test should be used to diagnose an active infection.
Tests for H. pylori fall into two main categories: invasive and non-invasive. Invasive tests utilize endoscopy as the means to observe lesions and obtain biopsies for histology, rapid urease testing, polymerase chain reaction (PCR) assays and culture. Non-invasive tests include serology for H. pylori-directed antibodies, urea breath tests, and stool antigen tests.

 When simpler front-line non-invasive tests indicate that endoscopy would be beneficial, additional information can be gained during the endoscopic exam (9). In addition, patients that have alarm symptoms (vomiting, GI bleeding, weight loss) should be evaluated immediately and directly by endoscopy (3, 9). Biopsies are an important part of the procedure and must be taken from at least 3 sites within the stomach and duodenum because inflamed regions are often patchy (9).
When simpler front-line non-invasive tests indicate that endoscopy would be beneficial, additional information can be gained during the endoscopic exam (9). In addition, patients that have alarm symptoms (vomiting, GI bleeding, weight loss) should be evaluated immediately and directly by endoscopy (3, 9). Biopsies are an important part of the procedure and must be taken from at least 3 sites within the stomach and duodenum because inflamed regions are often patchy (9).